
The use of item response theory (IRT) measurement methods can facilitate an enhanced understanding of subscale scores over traditional methods.
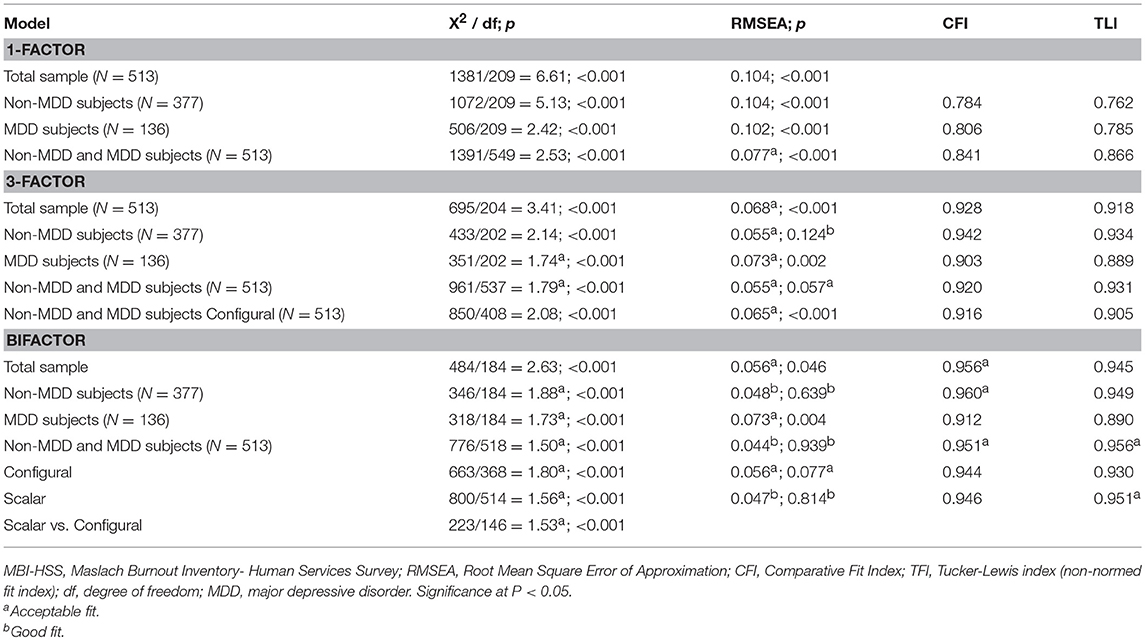
Traditional measurement methods do not permit users to directly compare subscale scores with the content of items to interpret their meaning.

One contributor to the observed inconsistencies in defining dichotomous burnout outcomes on the MBI may be the lack of clarity regarding the meaning of subscale scores. While the MBI is the most widely used physician burnout outcome assessment, a recent systematic review found a lack of consistency in cut-points used to define dichotomous burnout outcomes on each continuous MBI subscale, contributing to a marked heterogeneity in reported burnout prevalences across studies. Our results can be used to better understand the meaning and precision of MBI scores in US physicians compare individual/group MBI scores against a reference population of US physicians and inform the selection of subscale cut-points for defining categorical physician burnout outcomes.Ĭurrent US health policy discussions surrounding the physician burnout crisis have largely been informed by prevalence studies employing the Maslach Burnout Inventory-Human Services Survey for Medical Personnel (MBI). We produced a crosswalk mapping raw MBI subscale scores to scaled scores and response profiles calibrated in a US physician sample. Each subscale assessed the majority of sample score ranges with ≥ 0.70 reliability. At the commonly used EE and DP cut-points of 27 and 10, respectively, a physician was unlikely to endorse feeling burned out or any DP symptoms once weekly or more. The average US physician was likely to endorse feeling he/she is emotionally drained, used up, frustrated, and working too hard and all PA indicators once weekly or more but was unlikely to endorse feeling any DP symptoms once weekly or more. Response profiles were mapped to raw subscale scores and used to predict symptom endorsements at mean scores and commonly used cut-points. Using item response theory (IRT) analyses of secondary, cross-sectional survey data, we created response profiles describing the probability of burnout symptoms associated with US physicians’ MBI emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA) subscale scores. We described the burnout symptoms and precision associated with MBI scores in US physicians. Conclusions: The validity and reliability of this scale was established, enabling it to be used within the Portuguese population.Current US health policy discussions regarding physician burnout have largely been informed by studies employing the Maslach Burnout Inventory (MBI) yet, there is little in the literature focused on interpreting MBI scores. Convergent and divergent validation showed significant correlations. Pearson bivariate correlations were performed on the 150 participants, with an interval of 4 months for test-retest purposes with intra-class correlations from.
Maslach burnout inventory test professional#
These factors were emotional exhaustion (15 items), professional fulfillment (14 items) and depersonalization (7 items). Results showed 3 main components with 36 items explaining a total of 34.29% of the variance. Results: The initial 40 items were submitted to analysis for suitability of the data and 38 items were chosen for PCA. The psychometric methods used were exploratory factor analysis using principal components analysis (PCA), Cronbach’s α coefficients, and intra-class correlation coefficients. Method: The scale was validated with 280 HCWs working in oncology hospitals and in community home care in different parts of the country. The Burnout scale for workers who care for dying patients was created in 2005, by Gouveia Melo, using items from the Maslach Burnout Inventory (Human Services Survey) (Maslach, Jackson, & Leiter, 1997), the Burnout Test (Service Fields) (Jerabek, 2001) and items specifically designed for burnout in end-of-life care. Aims: The aim of this study was to develop an effective instrument to measure levels of burnout in Health Care Workers (HCWs) who care for dying patients and confirm the validity and reliability of the scale.


 0 kommentar(er)
0 kommentar(er)
